Compare your current eligibility and full breakdown benefit data against the actual payer portals and uncover hidden deltas, overcharges, and compliance risks in days
TruthCheck is a free audit engine that compares your insurance verification data with the actual information stored in payer portals. It uncovers mismatches that influence collections, compliance, patient liability accuracy, and overall operational performance.
Most organizations assume their eligibility and full benefit data is "close enough".
The reality we keep seeing:
Share a secure extract of your current verification data:
➤ Coverage Table, Frequencies
➤ Annual Max
➤ Or any data that you want to TruthCheck it
Our engine queries Payer Portals for the same patients, plans, and dates of service, treating them as the Single Source of Truth (SSOT).
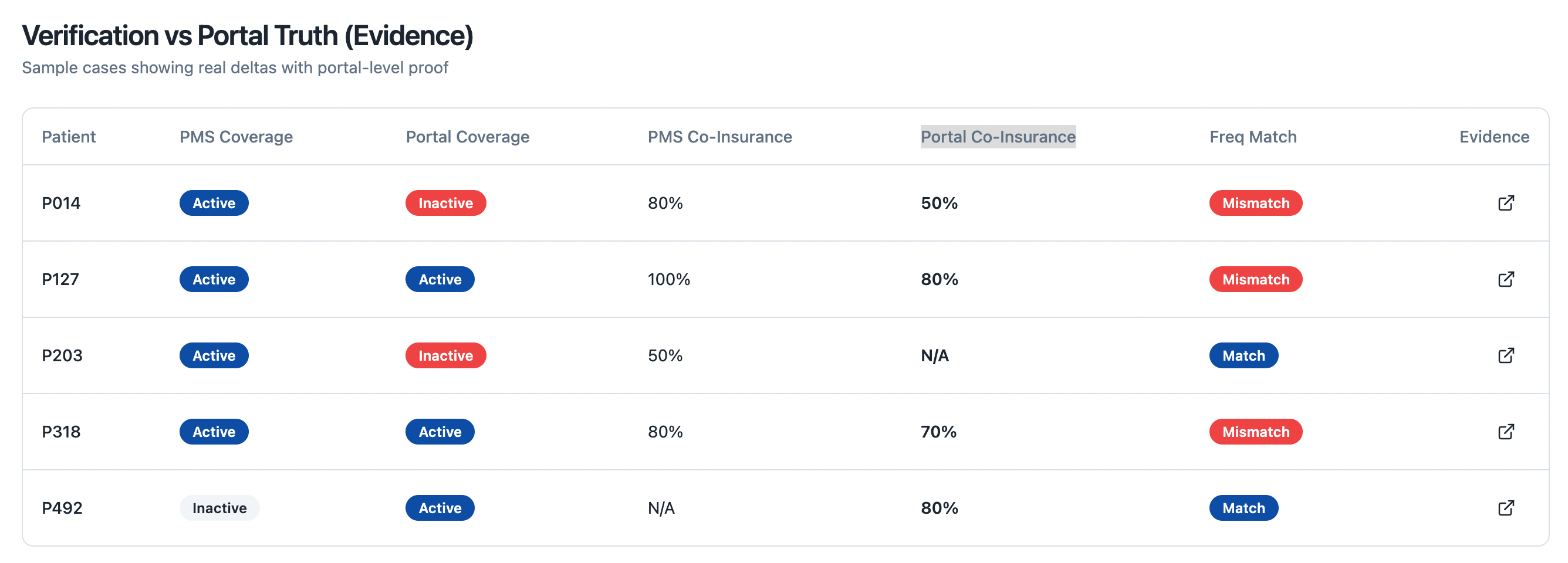
TruthCheck compares your values vs portal values for key fields like:
➤ Coverage status (active/inactive)
➤ Plan type & group
➤ Frequencies & limitations
➤ Copay, coinsurance, deductible
➤ Covered vs non-covered procedures
You receive a clear report showing:
➤ % of mismatched verifications
➤ Types of mismatches (eligibility, full benefit, frequency, coverage, etc.)
➤ Estimated patient overcharge exposure
➤ Priority payers / offices with the largest gaps
A short readout with your RCM, compliance, and finance leaders to walk through:
➤ Key findings
➤ otential legal & reputational impact
➤ Options to tighten your verification and data workflows
Comprehensive insights and actionable recommendations delivered to your team.
lorem
lorem
lorem
lorem
lorem
lorem